MIPS 2025 - Quality Reporting is Stricter Than You Think
Why EHRs will make or break providers’ MIPS scores this year, and what smart vendors are doing now
What’s Changed in the MIPS 2025 Quality Category
The 2025 changes to the MIPS Quality category are not just administrative updates. They directly affect how EHRs are built, how providers submit data, and how performance scores are calculated.
CMS has introduced new rules focused on data completeness, accuracy, and timeliness. These may seem technical, but the implications are far-reaching. Submissions that were once accepted with partial data can now be rejected entirely, making software infrastructure a much bigger part of MIPS success.
Here’s what’s new:
Every Quality measure must include at least one valid numerator and denominator
Missing required fields like Practice ID, Measure ID, Date of Service, or CMS EHR Certification ID will disqualify a submission
Three high-usage measures are now MVP-only: Breast Cancer Screening, Colorectal Cancer Screening, and BMI Screening
CMS will only score the most recent submission per collection type (Claims, eCQM, MIPS-CQM, QCDR measures) within an organization
More clinicians are exploring MIPS Value Pathways (MVPs) as CMS expands available options
These shifts demand new capabilities and better guidance from EHR vendors.
Why EHRs are in the Hot Seat
The 2025 MIPS Quality updates hit EHR vendors first. Your EHR now directly determines whether a provider's submission will be scored or thrown out. It’s no longer enough to passively support data entry and export. Your platform must actively guard against reporting errors.
1. Submission quality reflects product quality
EHRs must enforce front-end data validation. Incomplete or poorly structured files will lead to unscored measures, even if the provider delivered excellent care.
- Validate required fields like Practice ID, Date of Service, and Cert ID before allowing submission
- Flag incomplete measure entries with clear alerts
- Prevent users from submitting files with invalid or missing data
2. Measure libraries must stay current
Your users may unknowingly select disqualified or MVP-only measures. Without in-system guidance, their submissions could fail.
- Tag MVP-restricted measures and hide them from non-MVP workflows
- Recommend replacements based on the user’s specialty or reporting path
- Alert users when selected measures are no longer valid under traditional MIPS
3. Submissions must be trackable
CMS only scores the most recent submission per collection type within an organization. EHRs need to make submission history visible and prevent accidental overwrites.
- Log submission timestamps and track versions
- Notify users if a new file will overwrite a previous one
- Display submission status clearly within the platform
4. MVP support must be built in
MVPs are still optional, but they’re becoming the direction CMS is heading towards. EHRs that do not support them now will fall behind.
- Allow side-by-side view of MIPS and MVP options
- Let users filter measures by specialty and clinical focus
- Provide guidance for MVP onboarding and transition
What Healthcare Providers Must Watch For
While your EHR handles the technical components of MIPS, your internal strategy still needs to evolve. Success in 2025 will require more than trusting the system.
Your team needs to confirm that:
Your EHR and registry vendors are validating every required data field, including Practice ID, Measure ID, Date of Service, and CMS Certification ID
No retired or MVP-only measures are included in your reporting plan
Submissions are being reviewed regularly to avoid errors or accidental overwrites
Performance reviews are being done quarterly, not just at the end of the year
You have evaluated whether MVP pathways align better with your practice or specialty
Even with strong vendor support, these strategic checks can make or break your final MIPS score.
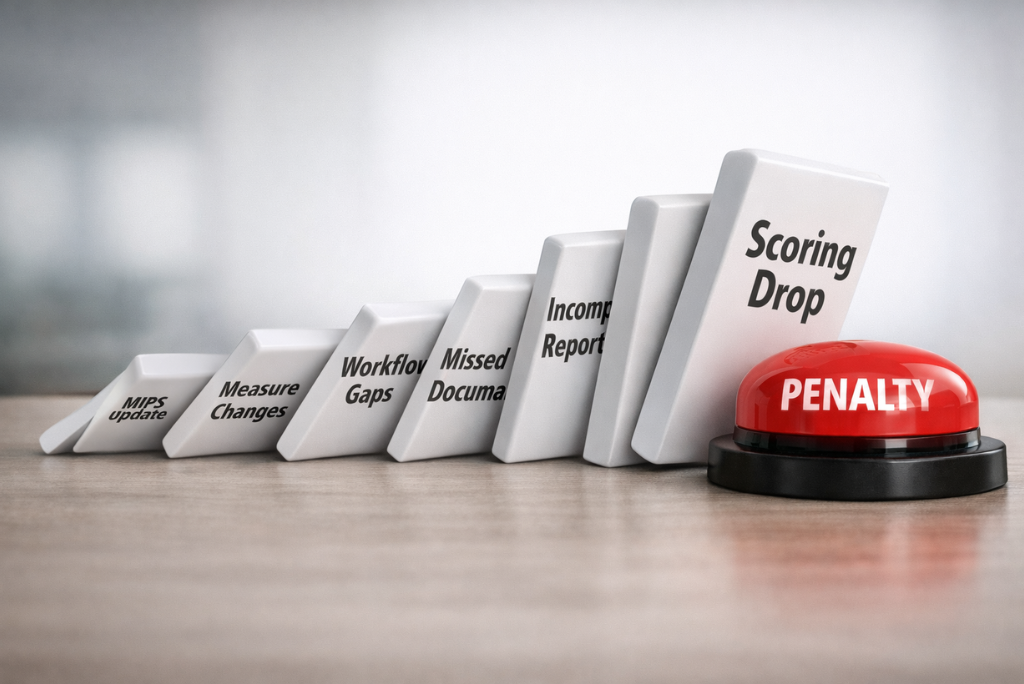
Why it Matters More Than it Seems
The Quality category still makes up a large share of the MIPS Final Score. CMS expects submissions to reflect not just accurate care, but clean and complete data.
EHR vendors who lag behind may cause their customers to miss out on bonus points or fall into penalty territory. Providers who trust their EHR without cross-checking may not even realize a measure was disqualified until it is too late.
This is no longer a once-a-year compliance task. It is an ongoing strategy with real revenue implications. It only works if the software infrastructure and clinical team are aligned from day one.
How Darena Health Helps You Stay in Compliance
At Darena Health, we help EHR vendors, Health providers, and Health organizations adapt to MIPS requirements without scrambling every year.
For EHRs , we provide certified components and backend services that support measure validation, data completeness, and flexible support for MVPs.
For providers, we offer Qualified Registry reporting through MyMipsScore, allowing for complete, compliant submissions even when internal tools fall short. We help identify measure selection risks early, surface eligible alternatives, and simplify the submission process without adding burden to clinical workflows.
We understand that MIPS reporting is not easy. But with the right tools and proactive guidance, it does not need to be a gamble.