MyMipsScore™
MIPS reporting made simple for EHRs, healthcare organizations, and provider groups.
What is MyMipsScore?
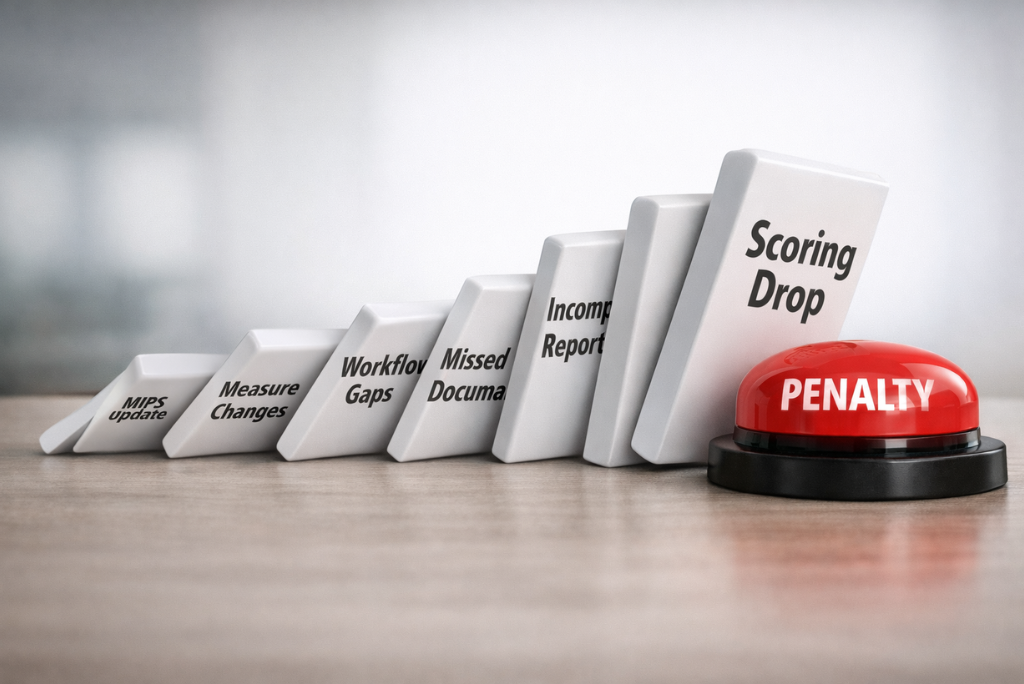
MIPS rules change constantly. Deadlines are strict, benchmarks shift, and reporting omissions and errors can lead to penalties. MyMipsScore is built to help with all of it. Designed for EHRs and health organizations, it offers a complete, CMS-ready solution for managing MIPS at scale.
With built-in functionality like MIPS score calculator, measure selection assistance, and direct submission to CMS, you can pick the most suitable Quality, Promoting Interoperability (PI), Improvement Activity (IA) measures, track performance, and stay audit-ready.
MyMipsScore supports EHR measures (eCQMs), Registry Measures (MIPS CQMs), and MIPS Value Pathways (MVP) reporting with low-lift integration and full compliance.
MyMipsScore gives you control without complexity to support providers for MIPS.
Why Choose Us?
Certified Modules
Plug-in modules for (c)(1-4) certification, Real World Plan and Test, and periodic attestations. Built for easy integration with commercial and homegrown EHRs.
MVP Ready
Supports all 21 MIPS Value Pathways (MVPs), all traditional MIPS measures, and custom reporting paths aligned with providers’ clinical focus.
CMS MIPS Registry
A CMS Qualified Registry since 2018. Supports all measures across Quality, PI and IA categories with updates, calculations, and submission.
Audit Support
Complete support for audits, targeted reviews, and Extreme and Uncontrollable Circumstances (EUC) filings. Data submitted stays audit-ready for up to 6 years.
All-in-One
One app for eCQMs, MIPS CQMs, and Claims measure selection, scoring, and submission across Quality, PI, and IA with specialty-specific guidance.
Easy Integration
User-friendly app with built-in dashboards, FHIR API support, and streamlined uploads. EHR integration is available for customers who need automated workflows at scale.
White Glove Service for MIPS 2026
Small provider groups often lack the time and resources to manage complex MIPS reporting. Our White Glove Service offers hands-on support to provider practices for selecting measures, tracking progress, and confidently meeting CMS requirements for MIPS.
We utilize MyMipsScore’s built-in measure simulator and MIPS score calculator to help you identify the right measures, avoid penalty, and improve your overall MIPS score. You focus on caring for patients. We handle the reporting.
If you'd like to simplify MIPS reporting for your group, reach out.
What is MIPS Score and Why it Matters
Your MIPS score is a number between 0 and 100 based on your performance in four categories: Quality (30%), Promoting Interoperability (25%), Improvement Activities (15%), and Cost (30%). Each category contributes a weighted portion to your final score.
If you bill Medicare Part B, your MIPS score directly impacts how much you get paid. The score you earn in 2026 determines your Medicare payment adjustment in 2028. Score 75 or higher to avoid penalties. A low score (<75) could reduce your payments by up to 9 percent. High scores (>75) can earn you bonus payments.
MyMipsScore supports both traditional MIPS and MIPS Value Pathways (MVPs), giving you flexibility in reporting and optimizing your performance.
Your 10-Step MIPS Guide
MIPS is now more demanding, not just for providers but also for EHR vendors and health organizations managing reporting at scale. The rules within each category have changed, measure requirements are stricter, and audit risks are higher. Certification needs, quarterly attestations, and PI requirements demand a system-level readiness. One misstep in measure selection, data used for measure calculation, or submission can mean lost points and thus penalties.
To help you get it right, we’ve created a practical 10-step guide that simplifies MIPS reporting, scoring, and submission for reporting using traditional MIPS and MIPS Value Pathways (MVPs).
Step 1: Reporting Track and Mode
Choose between Traditional MIPS, MIPS APM, or MVP. Your reporting mode - individual, group, or facility - affects your score setup.
LEARN MOREStep 2: Quality Measure Selection
Pick 6 Quality measures, including 1 Outcome or High Priority. Specialty sets are optional but may simplify selection.
LEARN MOREStep 3: IA Special Considerations
Small or rural practices need fewer activities. IA options vary based on size, TIN structure, and reporting method.
LEARN MOREStep 4: IA Scoring Rules
IA counts for 15% of your score. Groups must have at least 50% of NPI clinicians complete activities for 90 days.
LEARN MOREStep 5: PI Exceptions and Exclusions
PI may be reweighted to 0% for some clinicians. While certain measures allow exclusions, others must be reported to get a valid PI score.
LEARN MOREStep 6: Promoting Interoperability (PI) Scoring
Use an HTI-1 Certified EHR for 180+ days. Claimed exclusions affect scoring. Incomplete submissions often lead to low or no PI score.
LEARN MOREStep 7: Cost Category Measures and Scoring
Cost is 30% of your score. No data submission is needed - CMS uses claims. Measures depend on patient volume and eligibility.
LEARN MOREStep 8: Quality Weight and Measure Selection
Quality counts for 30%. If PI is reweighted, it may go up to 40%. Submit exactly 6 measures, including 1 Outcome or High Priority.
LEARN MOREStep 9A: Quality Measure Data Requirements
Each measure needs 75% data completeness and 20-case minimum. Use current-year specs for eCQMs. Missing either threshold results in 0 points. Choose wisely to avoid wasting scoring opportunities.
LEARN MOREStep 9B: Quality Score Calculation
Each measure earns up to 10 points. Some are capped at 7. CMS awards improvement bonuses. Your total Quality score depends on performance, completeness, and bonus eligibility across measures.
LEARN MOREStep 10A: Final MIPS Score Calculation
The final MIPS score is a weighted average across 4 categories. If one is exempted, weights are redistributed. You must report at least 2 categories to receive a final score.
LEARN MOREStep 10B: MIPS 2027 Payment Adjustment
2025 scores determine 2027 Medicare payments. Score under 18 gets a -9% cut. Under 75 still faces penalty. Higher scores receive positive adjustments. Max reward or penalty remains at 9%.
LEARN MOREMIPS Blogs
Trusted by
















































User Testimonials
Michael Goforth
EHR Implementation Director at Professional Imaging PLLC
"As an EHR Self Developer, partnering with Darena has made all the difference in our ability to keep up with the constantly shifting goal posts of the ASTP/ONC certification requirements. We are utilizing both their MyMipsScore and Darena Health applications for our practice and couldn't be more satisfied. Darena's products, consummate expertise and professionalism have made it far easier for us to manage our practice needs while remaining confident in our regulatory status."

Merced Gonzales
Chief Information and Technology Officer, HNI Healthcare
"Working with Darena has been great for our organization. Their tools and platforms have significantly reduced our administrative burden of MIPS compliance reporting, allowing our team to focus more on delivering quality care and less on navigating regulatory complexities. They are a Partner that truly understands the evolving landscape of healthcare and have consistently provided us with actionable insights, elevated our teams performance, and given us the support and confidence in meeting our MIPS requirements. On top of that, Darena’s responsiveness and commitment to our success have made them a trusted partner and I highly recommend Darena to any organization looking to streamline their compliance efforts with a partner that delivers both innovation and integrity."
Partner with us for (c)(1-4), (g)(10), (b)(11) and more
Darena Health has been a leading expert in healthcare IT regulation for nearly 15 years, helping EHR vendors, health IT developers, and healthcare organizations meet the 21st Century Cures Act, HTI-1, and the Quality Payment Program (MIPS) certification requirements.
Many of these requirements covering Information Blocking, FHIR APIs, and Promoting Interoperability (PI) MIPS category overlap in ways that create operational and technical complexity. We understand how these pieces fit together and can help you meet the criteria efficiently and accurately.
If you’re building toward compliance, we’re ready to support you.