MIPS 2025: Cost Category Insights
Claims-Based, Unforgiving, and Harder to Influence than You Think
A simpler framework, but no room for sloppiness
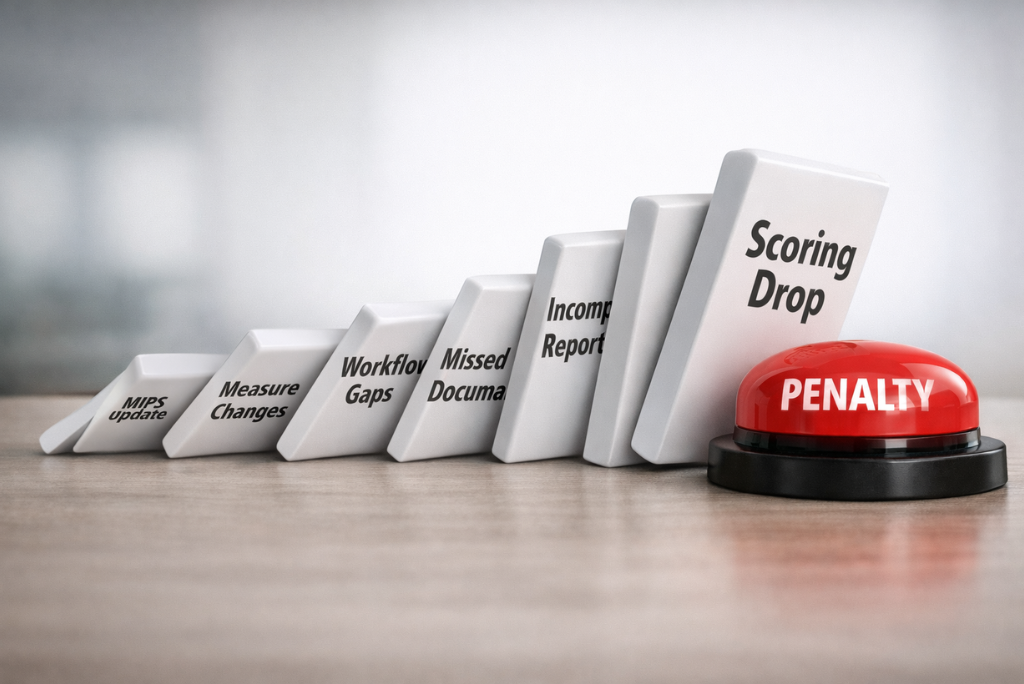
The Cost Performance Category may not require manual submission, but it is far from passive. For 2025, CMS is significantly expanding its oversight, adding new cost measures and tightening policy around performance exclusions. These changes can silently affect your score if you're not paying attention. Organizations that assume they’re safe just because claims are submitted will risk a harsh reality at the year-end.
Note: This blog is part of our MIPS 2025 series that covers all significant changes across categories: key MIPS 2025 updates and how to approach Quality reporting, Promoting Interoperability and Improvement Activities. Together, they help providers and EHRs prepare comprehensively for the evolving requirements.
What is the Cost Category?
The Cost category makes up 30% of your final MIPS score in 2025. It measures the total cost of care provided to Medicare patients, based on claims data - no separate submission is needed. CMS automatically calculates this score using measures like:
Total Per Capita Cost (TPCC)
Medicare Spending Per Beneficiary (MSPB)
Episode-Based Cost Measures tied to specific conditions or procedures
Cost performance is compared to national benchmarks, and even small gaps can lead to penalties. Unlike other MIPS categories, you can’t opt out or fix it after the fact.
What’s New: Six Cost Measures Added
CMS has added six new episode-based cost measures to capture spending across both acute and chronic conditions. These measures are designed to fill long-standing gaps in specialty cost tracking and ensure more consistent financial accountability across care settings.
Respiratory Infection Hospitalization
Chronic Kidney Disease
End-Stage Renal Disease (ESRD)
Kidney Transplant Management
Prostate Cancer
Rheumatoid Arthritis
Why it Matters
Even if your practice was previously untouched by cost metrics, this expansion could bring you into CMS’s scoring lens. A broader scope means more clinicians will have cost scores tied to their performance and claims history.
Pro Tip
Don’t wait until feedback reports show a dip. Review these measures now and identify which patients, services, and billing patterns could impact your score. Align care management and documentation accordingly.
Cost Measure Exclusion Policy Has Changed
CMS now allows certain cost measures to be excluded if significant anomalies exist in the data or methodology. This is not automatic and depends on your ability to demonstrate that scoring would be unfair or invalid due to specific events during the performance year.
Why it Matters
While this is a positive move, it shifts more responsibility to you, providers. Without internal monitoring and data traceability, you will not be in a position to use this exclusion pathway effectively.
Pro Tip
Treat every measure as potentially scoreable unless officially excluded. Set up alerts or checkpoints when claim trends deviate from clinical norms, and document any system-level issues that could justify exclusion.
Passive Reporting, Active Responsibility
Cost scores are calculated directly from your submitted Medicare Part A and B claims. There is no interface, attestation, or opportunity to clarify context after the fact. Your only control is the care you deliver and how you bill it.
Why it Matters
You cannot improve what you do not measure. CMS uses consistent benchmarks and risk adjustments, but if you are not tracking those metrics internally, your Cost score becomes a black box.
Pro Tip
Run retrospective analyses on high-cost episodes and chronic care trends within your claims data. Pay close attention to coding accuracy, complications, and readmissions, which all weigh heavily in cost scoring.
Cost Category = 30% of Your Final Score
The Cost category amounts to 30% of MIPS final score. It carries the same weight as Quality yet often receives far less operational attention. This imbalance is increasingly risky as Cost scoring gets more specific.
Why it Matters
A weak Cost performance can quietly undermine your entire MIPS strategy. Even perfect Quality or PI scores may not be enough to offset a poor showing here.
Pro Tip
Use multi-category scoring tools to simulate your MIPS final score under different cost performance scenarios. Identify which episodes or conditions are most likely to move the needle and focus your efforts there.
Summary: Cost is Quiet, but Critical
Because there are no alerts, submissions, or dashboards, Cost is often overlooked. But CMS is watching every Medicare claim. What you bill, how often, and with what outcomes are all visible, whether you’re paying attention or not.
Why it Matters
Unanticipated penalties are more dangerous. In many cases, the organizations that ignore Cost are the ones who have the most to lose. Financial stewardship is no longer optional.
Pro Tip
Make sure your Cost strategy includes a regular feedback loop. Look at claims, track costs across patient types, and bring finance and care management together. This is not just a regulatory box to check. It is a strategic opportunity.
How MyMipsScore can support you
Darena Health’s MyMipsScore™ helps you understand exactly what CMS evaluates in the Cost category. We keep you informed about which episode-based measures could apply to your practice based on your specialty, the case minimums, and the data sources CMS will use for a particular measure. With CMS-aligned logic and a unified view of all MIPS categories, you can act early and confidently. Be vigilant. You need to self-monitor, but we're here to guide you.
Ready to Strengthen Your MIPS Reporting?
Need help submitting MIPS? We support all four categories - Quality, Cost, Promoting Interoperability, and Improvement Activities.
Contact us to stay compliant and ahead in 2025.