MIPS 2026 changes look small, but could disrupt your operations
The 2026 MIPS Final Rule introduces a series of targeted updates that will affect how systems calculate, attribute, benchmark, and attest. None of them requires a major overhaul in your current processes, but several of them do require disciplined updates. While each change may appear incremental on its own, together they create a domino effect where small gaps in logic, documentation, or configuration can compound into measurable scoring impact.
To name a few, Claims-based Quality benchmarking is changing. Cost attribution logic has been refined. MVPs continue expanding into new specialties. Promoting Interoperability now includes dual security attestations that can zero out the entire category if mishandled.
For EHRs, this translates into logic adjustments, workflow validation, and careful roadmap planning. For providers, it affects timing, documentation, and specialty alignment.
The 2026 rule is not disruptive; it is precise. Precision creates operational responsibility. Read along to know more about the major changes.
Performance threshold and reporting paths
The performance threshold remains at 75 points and will remain there through the 2028 performance year.
For many practices, 75 is not a comfortable cushion. A few points gained or lost in Quality benchmarking, Cost attribution, or Promoting Interoperability can determine whether they avoid a penalty or fall below the neutral payment adjustment. There is limited room for error.
That reality affects EHRs directly. When customers are operating close to the threshold, they rely on accurate measure calculations, realistic performance projections, and submission workflows that do not create preventable scoring issues.
The three reporting paths continue:
Traditional MIPS
APM Performance Pathway (APP)
MIPS Value Pathways (MVPs)
MVPs remain voluntary, but CMS continues to expand and refine them. As the number of MVPs grows and becomes more specialty-specific, EHRs that support multiple specialties will need clearer measure alignment and configuration support, even if many customers remain in Traditional MIPS today.
MVPs are growing in importance
MVPs were designed to make MIPS more specialty-focused and clinically relevant. Instead of building a custom mix of measures, clinicians report within a defined pathway aligned to their specialty.
For EHRs, that structure can simplify configuration. But it also reduces flexibility. Measure mapping and specialty alignment must be accurate from the start.
2026 MVP expansion
For 2026, CMS finalized:
6 new MVPs
21 modified MVPs
27 total MVPs
New MVPs include Diagnostic Radiology, Interventional Radiology, Neuropsychology, Pathology, Podiatry, and Vascular Surgery.
If your EHR supports these specialties, MVP alignment becomes a current roadmap priority, not a future consideration.
Specialty self-attestation
CMS will not infer specialty from claims data. Groups must now self-attest their specialty composition during MVP registration.
This reduces CMS-side assumptions but shifts responsibility to the organization. EHRs should clearly support specialty designation and accurate measure mapping to avoid misalignment.
Vendor support timeline
Registries and QCDRs received a one-year ramp-up period before being required to support newly finalized MVPs.
This helps with technical sequencing, but customers will still expect clarity on which MVPs are supported and when, especially when they are interested in utilizing an MVP. EHRs stand to benefit if they stay tuned in and are able to offer these MVPs readily to their customers.
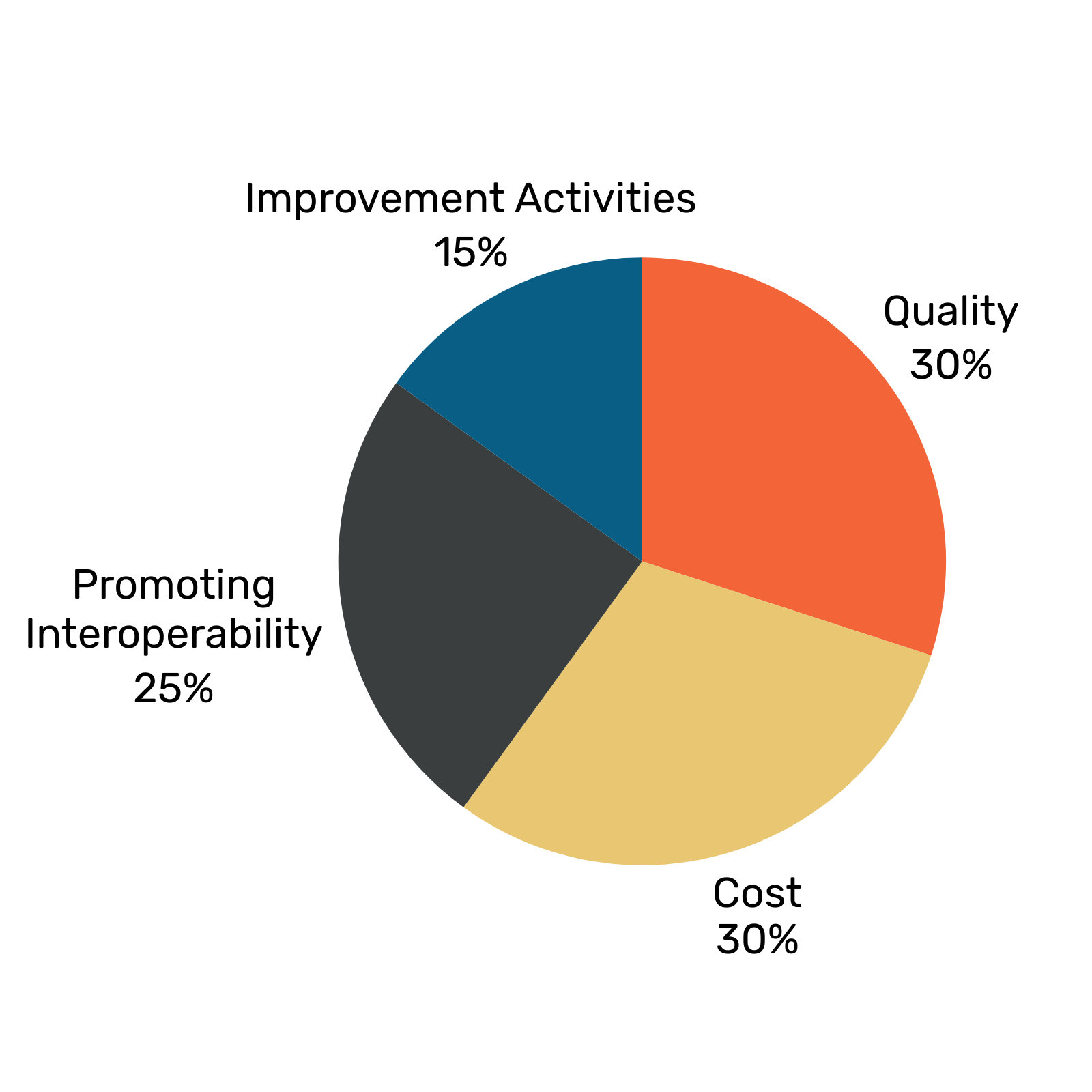
Category breakdown
Most of the 2026 updates sit within the individual performance categories. The structure remains the same, with scoring divided like this:
Quality- 30%
Cost- 30%
Promoting Interoperability- 25%
Improvement Activities- 15%
The sections below outline what changed inside each category and how those updates may affect reporting logic, documentation requirements, and scoring outcomes.
1. Quality Category: measure updates and new benchmarking logic
The Quality category evaluates clinical performance across selected measures, such as preventive care, chronic disease management, outcome rates, and care coordination. It accounts for 30% of the final MIPS score, making it one of the two largest scoring components.
For 2026, CMS reduced the total number of available Quality measures from 195 to 190. The update includes:
5 new measures
10 removed measures
30 modified measures
EHRs need to review specification changes closely, especially where measure logic, reporting criteria, or data capture requirements were modified. Even small changes to definitions can affect numerator and denominator calculations.
CMS also finalized a new benchmarking methodology for claims-based Quality measures. Instead of using the prior scoring distribution approach, benchmarking will now align more closely with Cost category scoring, using median-based comparisons and statistical cutoffs.
This has a practical impact. A practice could report the same clinical performance as in a prior year and still see a different score due to the revised benchmark calculations.
For EHRs, this affects performance dashboards, projected scoring estimates, and how results are explained to customers. Historical performance trends may not translate cleanly under the new benchmarking model, and expectations will need to be managed accordingly.
For providers, this means past performance is not a reliable predictor of 2026 scores. Measure selection and early performance monitoring become more important to avoid unexpected scoring shifts.
2. Cost Category: CMS-calculated and attribution-driven
The Cost category accounts for 30% of the final MIPS score. Clinicians do not submit data for this category. CMS calculates the score using Medicare claims data.
CMS assigns patients or episodes to clinicians or groups based on claims patterns. It then compares total spending for those patients against a national benchmark, adjusted for risk.
For 2026, CMS refined the attribution rules for Total Per Capita Cost (TPCC). The updated logic narrows how candidate events and related evaluation and management services determine which clinician or group is held responsible for a patient’s overall cost of care. The intent is to reduce attribution to specialists who may not have primary control over total spending.
No new cost measures were added for 2026.
CMS also finalized that any new cost measures introduced in the future will undergo two years of feedback-only scoring before they affect payment. During that period, performance will be visible but will not impact adjustments.
For EHRs, the key issue is alignment. Cost is calculated outside the EHR, but attribution logic affects which clinicians are scored and how performance is interpreted. Reporting tools and education materials should reflect the updated attribution rules.
For providers, the takeaway is straightforward: you cannot submit Cost data, but attribution and referral patterns still influence your score.
3. Promoting Interoperability: Security requirements carry full-category risk
Promoting Interoperability (PI) accounts for 25% of the final MIPS score. This category measures how clinicians use certified EHR technology for e-prescribing, health information exchange, patient access, and public health reporting. Clinicians report performance on required measures and attest to specific objectives to earn points.
The reporting measures remain largely the same, but CMS strengthened the security requirements.
For 2026, clinicians must attest to:
Conducting or reviewing a Security Risk Analysis (SRA)
Conducting Security Risk Management (SRM)
If either requirement is not met, the clinician receives zero points for the entire PI category. This eliminates 25% of the total MIPS score.
CMS also requires the use of the 2025 SAFER Guides under the High Priority Practices measure.
A new TEFCA-based public health reporting measure offers up to 5 bonus points when combined with other public health reporting measures.
Electronic Case Reporting is temporarily suppressed due to CDC onboarding limits. It must still be reported or formally excluded to avoid a zero score.
EHRs must support documentation and attestation for both the Security Risk Analysis and Security Risk Management. If workflows are unclear or incomplete, customers face direct scoring loss. PI is no longer just a reporting function. It is a compliance safeguard tied to a significant portion of the score.
Providers must ensure that both the Security Risk Analysis and the related Risk Management activities are completed and documented for the reporting year. Failure to do so turns the PI score to ZERO, regardless of performance on other PI measures.
4. Improvement Activities: updated inventory for 2026
The Improvement Activities category accounts for 15% of the final MIPS score and measures whether clinicians are engaging in efforts that improve care delivery, coordination, and patient outcomes. Clinicians select and attest to completing approved activities for a required period during the performance year.
For 2026, CMS added 3 new activities, modified 7, and removed 8. The prior Health Equity-focused activities were replaced with a new Advancing Health and Wellness subcategory. The structure of the category remains the same, but the available activity list has changed.
EHRs that support Improvement Activity tracking should update the inventory to reflect removed and modified activities and ensure that documentation requirements are clearly aligned with current CMS definitions. Outdated activity options can lead to incorrect attestations.
Providers should review their selected activities early to confirm they are still valid for 2026. If an activity has been removed or revised, a replacement will be necessary to avoid losing points in this category.
Fun Insight
The 2026 rule is not difficult to read. It is difficult to operationalize consistently.
Most scoring losses do not come from misunderstanding CMS policy. They come from small gaps in measure logic, missing benchmarking updates, failing to check for discontinued measures, attribution understanding, or incomplete documentation that go unnoticed until submission. At a 75-point threshold, those gaps matter.
In 2026, success will depend less on knowing the rule and more on maintaining disciplined execution across calculation, validation, and documentation throughout the year.
How Darena makes MIPS reporting less complicated
The 2026 MIPS updates require steady maintenance, as eCQM specifications change, MVP pathways expand, Quality measures and benchmarking logic shifts, security attestations carry full-category risk, and CMS submission rules remain strict.
MyMipsScore manages the responsibility in a structured way.
It supports all 2026 reporting paths, including all 27 MVPs, and handles calculation, validation, scoring, and CMS submission across Quality, Cost, Promoting Interoperability, and Improvement Activities. Instead of building and maintaining this infrastructure internally, EHRs integrate through secure APIs into a system that is already aligned with current CMS requirements.
MyMipsScore is ASTP/ONC Certified for (b)(10), (C) (1-4), covering eCQM recording, calculation, filtering, import, export, and reporting across all eCQMs (EHR measures). It is also certified under (d)(1-3,5,12,13) supporting access control, safety functionality, and audit requirements. This certification allows MIPS capability to integrate without disrupting an EHR’s existing certification structure.
As a CMS-Qualified Registry, MyMipsScore manages submission validation, file formatting, and CMS connectivity within an established infrastructure that is maintained year-round.
For EHRs, this reduces compliance burden on technical teams, limits recurring regulatory engineering work, and lowers submission-related risk. It also improves customer satisfaction by providing stable scoring, fewer reporting errors, and reliable submission outcomes, which in turn supports stronger customer retention and more predictable revenue tied to MIPS-enabled functionality.
The result is that annual MIPS updates are handled in a controlled and predictable way, reducing engineering workload and lowering submission risk.
What does this change for EHRs
Working with Darena shifts MIPS from a recurring engineering project to a managed capability. Instead of rebuilding logic and submission workflows each year, your team integrates with a structure that is already up-to-date with CMS requirements. Your EHR no longer needs to:
Maintain certification requirements for MIPS to support Promoting Interoperability and Quality measures internally.
Manage yearly eCQM specification updates and calculation logic within your own system.
Build and maintain full MVP coverage, including new and modified pathways.
Develop and operate CMS submission infrastructure, including validation and error handling.
Continuously update scoring and validation logic to keep pace with CMS changes and reduce reporting-season support burden.
With MyMipsScore, EHRs can support the full spectrum of MIPS for their customers without bearing the burden of all the above-mentioned tasks annually. This allows engineering teams to focus on product priorities rather than annual regulatory maintenance.
What does this change for Providers
For providers, especially small and mid-sized groups, MIPS reporting often becomes rushed near deadlines. Our White Glove Service provides structured, year-round support, enabling performance to be monitored early and adjusted as needed.
MIPS reporting track selection – MVP evaluation if applicable
Measure selection is guided based on specialty and scoring goals.
Performance is tracked throughout the year using score simulation tools.
Data gaps and documentation issues are identified before submission.
Security Risk Analysis and Security Risk Management requirements are tracked to prevent loss of the PI category.
By submission time, data is validated and organized, reducing avoidable errors and scoring surprises.